by Megan Aul, MA, LPC, Enterhealth Outpatient Center of Excellence Therapist
Dialectical behavior therapy (DBT) is an evidence-based form of psychotherapy developed in the late 1980s by Marsha M. Linehan to treat patients who didn’t respond well to traditional behavioral therapy (specifically those with borderline personality disorder). Since its development, DBT has also proven to be an effective technique for treating other types of difficult patients, including those with mood disorders, PTSD, eating disorders, substance abuse disorders and more.
DBT is a modified form of cognitive behavioral therapy (CBT) that focuses on creating a therapeutic alliance (that is, the patient sees the therapist as an ally rather than adversary) and helping the patient find a balance between acceptance of where they are and realization of the changes necessary to live a normal life. This is what the term dialectics refers to – the synthesis or integration of two opposites. In treatment, these opposite concepts include things such as emotion versus reason and acceptance versus change.
The main goal of DBT is to teach patients skills such as how to regulate their emotions, live in the moment, better cope with stress, and improve their relationships with others. Through individual and group therapy sessions (as well as other components we will discuss), DBT also teaches patients how and when to apply these skills to real-life situations and stressors.
The four skills of DBT
The skills taught in DBT fall into four main categories:
Mindfulness – Skills that focus on keeping the mind in the present, slowing down the thought process, and teaching patients to focus on caring for themselves without letting intense emotions lead them to destructive behaviors.
Interpersonal effectiveness – Skills that teach patients to recognize what they need in relationships and how to deal with other people and their needs in healthy ways.
Emotion regulation – Skills designed to help patients recognize and respond appropriately to their own emotions without becoming overwhelmed by them.
Distress tolerance – Skills aimed at helping patients develop healthy coping mechanisms and ways to deal with emotional stress that don’t include destructive behaviors or substance abuse.
The five components of DBT
In order to address some of the difficulties in treating resistant patients and to prevent therapists from becoming overwhelmed, DBT involves several therapeutic components:
Structured individual therapy – Weekly individual therapy sessions that prioritize skills acquisition and combatting the patient’s negative behaviors (e.g. life-threatening, treatment-interfering, quality-of-life behaviors, etc.).
Skills group therapy – Weekly group therapy sessions designed to help patients acquire new skills that promote acceptance (mindfulness, distress tolerance) and change (interpersonal effectiveness, emotion regulation).
Individual coaching – Conducted over the phone, this component focuses on helping patients deal with stressful situations that arise in their everyday lives as they happen in real time.
Treatment team (a.k.a. therapy for the therapist) – Weekly sessions in which the therapy team meets without patients to collaborate on patient care and ensure that all the therapists remain motivated and competent (DBT can be an intensive form of treatment both for the patient and the therapist).
Case management – This ongoing aftercare component ensures that patients are properly applying the skills learned in therapy to their everyday lives.
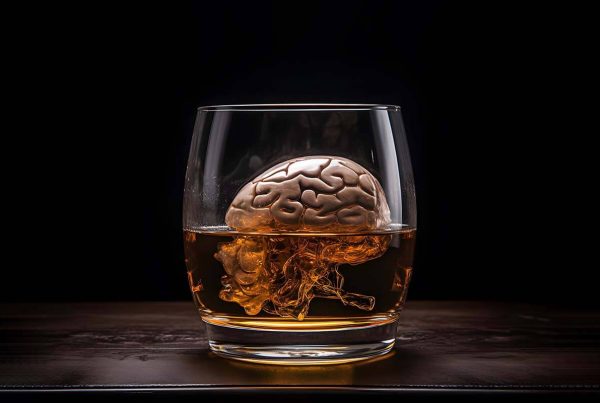
DBT and addiction treatment
Dialectical behavior therapy is particularly useful in a substance abuse treatment setting because many patients who enter treatment suffer from co-occurring psychological disorders, a condition referred to as a dual diagnosis.
Patients who suffer from these kinds of psychological dual-diagnosis conditions (mood disorders, PTSD, eating disorders, etc.) tend to have less emotional stability, which often leads to substance abuse as a coping mechanism for stress or as a way to self-medicate negative feelings. Because these patients can be difficult to treat using traditional methods, more and more addiction treatment centers – like Enterhealth – are turning to therapeutic modalities like DBT for help.
How Enterhealth uses DBT to improve patient outcomes
Since it was formed more than a decade ago, Enterhealth has embraced the use of evidence-based treatments and therapies. It’s for this reason that we offer services you won’t find at every treatment provider, including Medication-Assisted Treatment (MAT).
In addition, our therapists employ a range of techniques that includes Dialectical Behavior Therapy, Cognitive Behavioral Therapy, Motivational Enhancement Therapy, and Acceptance and Commitment Therapy.
Enterhealth’s true secret to success lies in our ability to create custom treatment plans for each patient. Through initial evaluations and interviews, our team of addiction-trained physicians and therapists are able to determine which services and therapies are most appropriate for each patient.
To learn more about Enterhealth and the benefits of proven, evidence-based treatments like DBT, call 1.800.388.4601 or contact us today.